A study published in Transfusion Medicine shares transfusion laboratory insights and challenges into red blood cell (RBC) inventory management. The authors of the paper explained that their study aims to, “provide complementary data to quantitative models that incorporate human factors in the inventory management of RBCs, particularly Group O negative RBCs.” The transfusion laboratory insights into inventory management study included interviews with 16 individuals, “with representatives from the same institution interviewed simultaneously in a focus group style conversation using the same semi-structured interview guide.”
The researchers noted their semi-structured interview guides were co-developed with technologists, technical leads, medical directors, and data analytics leads. Interviews occurred via Zoom from September to November 2022. The paper discovered that five themes impacted technologist decision-making on RBC inventory management:
- “[b]alancing logistics, local policies, and human factors in inventory management;
- [v]arying perceptions of redistribution and its unintended consequences;
- [g]uidance on the appropriate usage of O negative RBCs and management;
- [d]efining efficiency and the performance measures of inventory management; [and]
- [c]ultural barriers to inventory model integration in healthcare.”
The authors explained that their key takeaways from the transfusion laboratory insights into inventory management study included that the top three inventory practices are:
- [u]sing group O positive RBCs for emergency use;
- [r]edistribution and prioriti[z]ing fresher RBCs for rural/remote sites; [and]
- [t]ransfusion of O negative RBCs to typed non-O patients to avoid expiry.”
Their research also found that the challenges managing O-negative RBCS are:
- “the demand for O negative RBCs strains its supply, so that O positive RBCs are often used as substitute universal donor RBCs;
- predicting patient use;
- rural/remote sites historically do not use much inventory but need to be prepared for an emergency and often must carry group O blood because of lack of testing in those areas/lack of blood bank specific staffing;
- inventory is stockpiled, aged, and then used to avoid expiry;
- redistribution has the unintentional result of facilitating overordering;
- varying opinions of the optimal use of O negative RBCs; [and]
- changing clinical and inventory practices to help better manage O negative is difficult.”
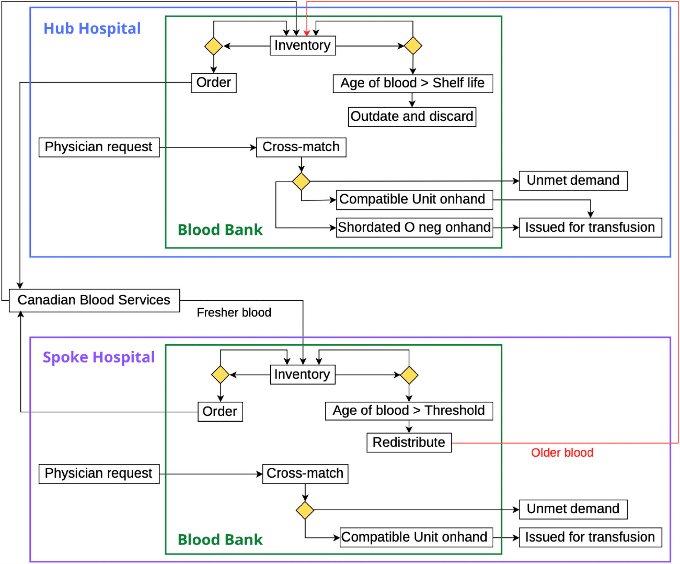
The authors used the findings to develop a flow chart of inventory management that they believe, “can be generali[z]ed to other jurisdictions [since it was built] to include a network of hospitals and redistribution of group O negative RBCs [and] is calibrated to real-world data and uses inventory management performance indicators identified from technologists and technical leads.” The researchers concluded that, “[t]hrough our qualitative methods, we have identified key factors for understanding practices in RBC inventory management for hospital blood banks catering to diverse needs across a jurisdiction spanning a large geographic area with numerous rural/remote patient populations. The insights [gained and reported] can inform appropriate inventory levels, ensuring equity in resource allocation for rural/remote blood banks with varying inventory usage.”
Citation: Dhahan, J., Morrison, D., Shih, A. et al. “Red blood cell inventory management: Insights from transfusion laboratory technologists in British Columbia, Canada.” Transfusion Medicine. 2025
